Programs designed to lower hospital readmissions often focus on patient characteristics associated with reimbursement penalties assessed by the Centers for Medicare and Medicaid (CMS). This approach makes a lot of sense because the Hospital Readmission Reduction Program (HRRP) only reduces payment for readmissions associated with certain diagnoses — acute myocardial infarction, heart failure, pneumonia and several other conditions.
In this article, we will tackle the structural factors that lead to the highest penalties under the HRRP, and how to overcome the challenges associated with these factors by accessing physician specialists using telemedicine.
Community, Structural and Performance Factors
Since 2012, the first year that reduction in CMS payments were imposed, several studies have evaluated the community and facility characteristics most likely to influence the 30-day Risk-Standardized Readmission Rate (RSRR).
Researchers have considered everything from ownership to metropolitan status to bed size. What’s clear is that some structural factors play a greater role in readmissions according to a study published by Jason N. Mose and Neela K. Kumar in Health Equity. Risk of readmissions are higher if your hospital falls into one or more of these categories:
- Medium or large hospital
- For-profit and teaching facilities
- High average occupancy
- Serves a community with high Emergency Department utilization and/or high comorbidity rates
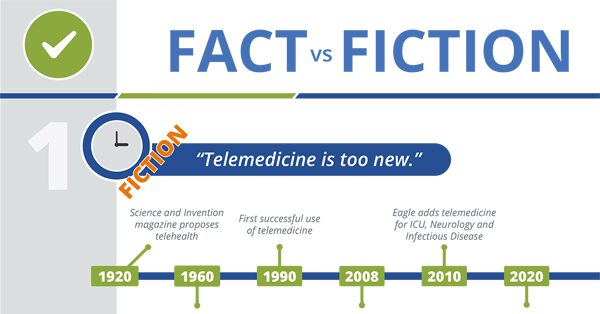
Telemedicine and Healthcare – What’s Fact and What’s Fiction?
The good news is that these categories have changed over time. Immediately following the launch of the HRRP, high penalties were more common among rural hospitals. In addition, a significant portion of hospitals in all of these categories received little or no penalty for readmission. Both of these factors suggest that changes within the facility can impact your hospital’s risk of receiving a penalty.
It’s more difficult to parse the geographic regions that most impact readmission rates. However, studies published by the Robert Wood Johnson Foundation and Upper Midwest Rural Health Research Center, demonstrate that:
- Prospective Payment System (PPS) rural hospitals and Critical Access Hospitals in New England, Mid-Atlantic and Pacific regions have lower readmission rates than urban hospitals
- Southern PPS rural hospitals and CAHs experience higher readmission rates than urban hospitals in the same region
Do these findings mean community, structural and performance factors doom some facilities and protect others from penalties? Of course not. However, reviewing your facility’s characteristics in light of this information can highlight what actions will reduce 30-day readmission rates.
Follow the data to find a solution to hospital readmissions
In the first article in our discussion of hospital readmission reduction programs, we focused on how improved diagnosis and prescription selection can reduce 30-day readmissions. In the blog Reduce 30-day readmission rates by accessing specialist consults in the ED, we covered how accessing specialists can prevent unnecessary readmissions thru the Emergency Department.
Now, let’s consider how a consult with a specialist can offset the factors that put some facilities at great risk of readmissions. In the Mose and Kumar study cited above:
“Taken together, structural, performance, and community factors are important in explaining variation in the likelihood of receiving a penalty… there is room for providers to reduce avoidable readmissions and policymakers to mitigate unintended consequences.”
How to reduce avoidable readmissions?
An in-person or telemedicine consultation with a specialist can help your hospital avoid premature discharge and improve admissions decisions in the ED. In addition, specialists can help reduce clinical factors that are highly correlated with readmissions, including:
- Use of high-risk medications
- Comorbidities
Community factors, like high ED utilization, can also be addressed by accessing a specialist.
Premature discharge from the hospital
Treatment of COVID has raised awareness about the need for specialist consults when hospital staff and physicians are approaching burnout.
“Before COVID there were benefits to consulting an infectious disease provider. After COVID, it’s [consulting an infectious disease physician] even more important,” says Dr. David Fitzgerald, Infectious Disease Specialist and Tele-ID provider at Eagle Telemedicine. “Doctors on the frontline are really stressed and stretched. I hear it in the voices of the residents that are calling me. Instead of just one ICU full of COVID patients, they now have two ICUs full of COVID patients. It’s also helpful because a lot of these institutions only have one or two infectious disease doctors. Telemedicine lets these doctors focus on the COVID patients.”
Hospitals with high average occupancy rates may benefit from consulting with specialists, like Dr. Fitzgerald, long after the coronavirus is under control. These hospitals experience patient demand for care that tax hospital staff for extended periods. Engaging with a TeleCardiologist, TeleNeurologist, or TelePulmonologist can provide Surge ProtectionTM when the ED is overloaded or patient floors are nearing capacity.
Can Better Diagnoses Help with Hospital Readmission Reduction Program Initiatives?

Use of high-risk medications
The study Redefining Readmission Risk Factors for General Medicine Patients published in The Journal of Hospital Medicine identified two types of medications, steroids and narcotics, associated with higher readmission rates. Consulting another physician can help minimize drug interactions and add insight into what medications are truly necessary after discharge. Adverse drug event (ADE) errors are common and costly.
Abuse and misuse of medication as well as medication non-compliance are factors that contribute to readmission risk. Minimizing the number of medications a patient is on at the time of discharge is one way to lower the risk of side effects and drug interactions that may trigger a return to the hospital for additional care. Medication reconciliation, comparing a patient’s medication orders to all of the medications that the patient is actually taking, is another way to minimize medication-related complications and improve quality of care.
Comorbidities
In patients with comorbidities, the reason for readmission is often unrelated to the original hospitalization. Identifying patients with comorbidities and proactively coordinating care with their existing specialist or consulting with a Specialist can help hospitals reduce admissions by identifying how treatment and discharge for one condition may impact other health issues.
The treatment of comorbid patients is one possible reason that medium and large hospitals have higher readmission rates and, therefore, higher HRRP penalties. These facilities may also have higher average occupancy rates because larger hospitals operate in more densely populated areas, serve lower socioeconomic communities and receive transfers from the smaller hospitals – leading to treatment of sicker patients with more complex conditions.
High ED Utilization
High utilization of the ED is often associated with the use of the hospital for primary care services. This metric may also signal a lack of access to primary care. Focusing on the admission interview can identify underlying health issues or previously undetected comorbidities that need to be addressed during the inpatient stay and require outpatient coordination. Awareness of these conditions and the need for follow-up care that is unrelated to the inpatient stay can lower the risk of readmission.
To avoid HRRP payment reductions, hospitals should look at community, structural and performance factors as well as clinical care to build a comprehensive plan. Using telemedicine strategically can complement efforts to expand patient access and reduce hospital readmissions. In our final article on the topic of HRRP, we discuss how hospital patient transfer can impact your hospital’s reimbursement.
Read more about how telemedicine can reduce readmissions:
- Can better diagnoses, prescriptions help with hospital readmission reduction program initiatives?
- What’s the impact of physician burnout on readmission rates?
- Can hospitals reduce 30-day readmission rates by accessing specialist consults in the ED?
- Will improved discharge procedures lower hospital readmission rates?
- Can reducing hospital patient transfer lower readmission rates?







