Nurse Practitioner, Rebecca Carter at Anthony Medical Center in Kansas say: “I couldn’t do what I do without them.”
That’s how one Nurse Practitioner at a critical-access hospital in rural Kansas sums up the backup support she gets from hospitalists in the Eagle Telemedicine program at her facility. Rebecca Carter, APRN, was a champion of the telemedicine program when it began at Anthony Medical Center (AMC) in Anthony, KS, in January 2015. Today, nearly three years later, she is a stronger champion than ever.
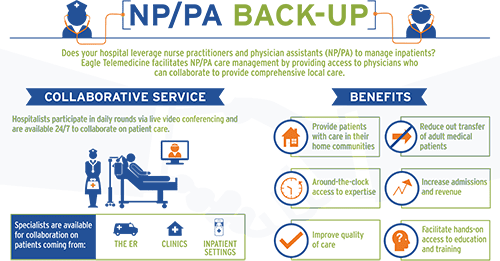
In previous blogs, we’ve written about the big-picture benefits of telemedicine for rural hospitals: solving staffing needs; helping nurse practitioners and physician assistants move into leadership roles in clinical settings where physicians might be hard to find; and reducing the number of patient transfers to tertiary facilities.
So, we thought it was time to feature a personal perspective. In AMC’s inpatient facility, its Emergency Department (ED) and its attached rural health clinic, our telemedicine program provides backup support for Carter, three PAs, and a new NP who recently joined Carter and the team at the 25-bed hospital. By providing guidance and confirming the decisions these healthcare professionals make, the telemedicine program also supports the three physicians—one full-time and two who visit one or two days a week—who staff the facility.
All of them view the telemedicine program as an essential part of the healthcare team at AMC. Carter graciously agreed to share her own experience for this blog post—how the program has helped AMC patients and enabled her to be a more confident, more knowledgeable healthcare professional.
Taking Nurse Practitioner Knowledge to a New Level
Like many NPs, Carter was certified as a family nurse practitioner when she became an nurse practitioner 12 years ago. She was qualified to work in family-practice clinics, but didn’t have training in the acute care setting. But in her nursing work in an ED at a large hospital in Wichita and in other settings, she gained the inpatient experience she needed to accept a position at AMC nearly 10 years ago.
At that time, AMC had contacts with several inpatient specialists in Wichita who would provide nurse practitioners and physician assistants with expert opinions when needed. But when the Eagle Telemedicine program began and its hospitalists became immediately available to the team, the backup process became more structured, more comprehensive, more consistent, and more effective.
“When Eagle came on board, we could discuss each of our patients with their TeleHospitalists and look at our patients from a broader perspective,” Carter said. “We transfer fewer patients because we make more confident decisions that patients can stay here with our own resources and get the level of care they need. The telemedicine program has really expanded my scope and taken my knowledge base to a new level.”
Combines Video, Phone and Text
Carter estimates that the telemedicine cart with built-in two-way videoconferencing and diagnostic tools is used about 20 percent of the time nurse practitioners and physician assistants need support from the Eagle team, with the other 80 percent of contacts occurring via telephone conversations and occasionally texts for sharing information that is not confidential and not patient specific. Carter relies on this backup support by telephone in her work in the inpatient setting, especially on morning rounds, and in the ED when making decisions about admitting patients.
Typically, NPs and PAs at AMC do initial assessments of patients with the backup support of the TeleHospitalist team, which has access to patient electronic medical records (EMRs). If there are questions, a TeleHospitalist might “beam in” via videoconferencing to make his or her own assessment. The videoconferencing cart is also used at the point when Medicare requires a physician’s evaluation for a patient to move from the acute care level to the Skilled Nursing Facility (SNF) level of care at the facility. AMC has 25 beds, and all beds are certified for acute and/or “swing beds.”
Whatever the communication medium, Carter finds the TeleHospitalist support invaluable to do her optimal clinical performance. She tells the story of a young patient who had overdosed and was brought to the ED in cardiac arrest. “While we were providing resuscitation for the patient, I discussed the patient’s condition and considered all potential causes with Dr. Jason Kimball, one of the Eagle TeleHospitalists in Lawrence, Kan. We did have to fly the patient out, but he is alive today. I believe we had that outcome because we were working in conjunction with Dr. Kimball on a very complicated clinical case.”
“Where the future is going”
Working to obtain her Doctorate of Nursing Practice degree from Wichita State University in 2018, Carter describes herself as a “lifetime student” who appreciates the confirmation and validation she gets from Eagle’s TeleHospitalists, even when she knows the answer to the questions she asks them. “Their positive feedback is invaluable,” she said. “They respect me. There have never been any disrespectful interactions. The doctors are phenomenal.”
Occasionally, Carter will use the videoconferencing cart if families want to speak directly to a physician, but as the years go by, the community has become familiar with the telemedicine program. They request that contact less and less frequently. “They are very comfortable with our hospital providing the level of care their loved ones need,” she said. “Telemedicine is where the future is going. I can’t speak highly enough of it.”







I was really happy to see that you mentioned you are basically a lifetime student. Medicine is always advancing and is always developing something new. This aspect of the nursing field is a really great appeal to me. I am always wanting to learn as much as I possibly can. Thank you so much for sharing this great information. As I decide what major to take I will keep this in mind.
Thank you for reading the Eagle Telemedicine blog. Rebecca Carter is such a shining example for nurse practitioners advocating for and participating in telemedicine’s expansion in the healthcare field.