COVID-19 put the spotlight on telemedicine for pulmonology. However, hospitals see their share of chronic non-COVID respiratory disorders on a regular basis. Many of these patients are in and out of hospitals for years, as their condition progresses.
It’s a burden for small community, rural or inner-city hospitals, trying to provide the specialist care these patients need. The unpredictability of these hospitalizations typically means referring the patient to a tertiary care hospital, often up to 100 miles away.
Patients find it very stressful, and in some cases impossible, to make that trek when suffering with a respiratory condition. If they are turned away from their local hospital, they likely won’t seek treatment there again — meaning that revenue is lost forever. This diminishes the hospital’s reputation in their community, as word gets around they just can’t handle “serious” patients.
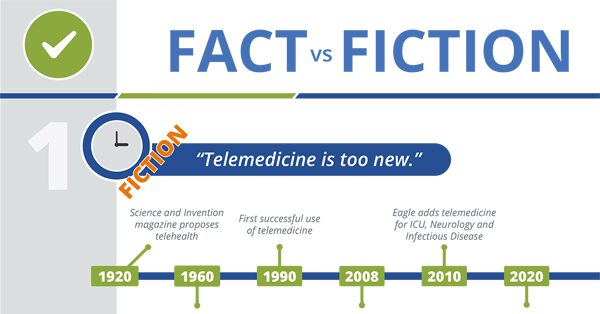
Telemedicine and Healthcare – What’s Fact and What’s Fiction?
With Eagle pulmonology telemedicine, hospitals get the support they need in managing these chronically ill respiratory patients. Telehealth providers take the pressure off staff doctors by treating the immediate issues as well as developing a long-term care plan.
If the patient requires ICU-level care, the TelePulmonologist can jump into that role, which is why we offer Tele-ICU services, says Talbot “Mac” McCormick, MD, CEO of Eagle Telemedicine. “For smaller hospitals without an ICU, the TelePulmonologist works closely with on-site staff who perform invasive procedures when intubation or ventilator care is needed.”
“Eagle’s TelePulmonologists can manage ventilator care, Code Blues, run an ICU and handle daily patient rounds on the hospital floor,” explains Dr. McCormick.
With access to TelePulmonology, patients are able to get high-level specialist care in their hometowns. “It’s comforting for patients and their families, and rewarding for on-site hospital staff wanting to provide optimal medical care,” Dr. McCormick says.
“The hospital’s reputation is enhanced when patients get multi-disciplinary specialist care at their community hospital,” he adds. Patients develop a higher sense of security in their healthcare, and the community in general benefits from the enhanced medical resources. The hospital’s financial picture also improves greatly, and the community’s economic base stabilizes.
Chronic respiratory disorders telemedicine for pulmonology can handle:
Asthma
In the ambulatory and emergency department settings, treatment aims to correct severe asthma exacerbations, hypoxemia, rapid reversal of airflow obstruction, and reducing risk of relapse.
Systemic corticosteroids administered within one hour of ER admission decreases the need for hospitalization, especially in patients with severe exacerbations. Airway inflammation can persist after an acute attack, so more intensive treatment may be necessary.
Telemedicine for pulmonology requires remote pulmonologists to draw on evidence-based research in outlining treatment for patients — including even the most serious exacerbations.
Chronic Obstructive Pulmonary Disorder
Patients with COPD typically have both emphysema and chronic bronchitis, but the severity of each condition varies. People with asthma can also develop COPD, and severe symptoms may require emergency care and hospitalization.
If respiratory function continues to deteriorate despite hospital treatment, patients require admission to an intensive care unit for frequent respiratory status monitoring and possible ventilator assistance.
Eagle Telemedicine for pulmonology provides pulmonary critical care physicians that regularly work with COPD at all stages and is skilled in working closely with onsite teams performing invasive procedures. If the hospital doesn’t have an ICU, the TelePulmonologist can provide high-level treatment and consult with additional specialists as necessary.
Interstitial Lung Disease
Interstitial lung disease (ILD) refers to diseases that cause scarring (fibrosis) of the lungs, making breathing difficult. Lung damage from ILDs will worsen over time, and is typically irreversible. Patients with COVID-19 and ILD have increased risk of death.
Very often, substantial lung damage has occurred by the time a diagnosis is made. Severe cases left untreated can lead to life-threatening complications including high blood pressure, heart or respiratory failure.
A TelePulmonologist will recognize potential symptoms of ILDs very quickly, expediting on-site testing with x-rays, CT scan, lung function tests, bronchoscopy or lung biopsy. Guided by the TelePulmonologist, treatment will be specific to the ILD and the severity, focused on improving quality of life and slowing the disease progression — with the most appropriate medications, oxygen therapy and pulmonary rehabilitation.
Pneumonia
For some people, breathing problems associated with pneumonia can become severe enough to require hospital treatment with oxygen or even a ventilator. COVID-related pneumonia often takes hold of both lungs and is often severe, causing lasting lung damage.
Pneumonia can be hard to diagnose because symptoms are similar to a cold or flu, and patients may not realize the severity until they end up in the hospital emergency room. Older adults, infants and people with serious illnesses or weakened immune systems may not have typical symptoms.
Without accurate diagnosis and quick treatment, pneumonia complications can be life-threatening including acute respiratory distress (ARDS) and respiratory failure; kidney, liver, and heart damage, necrotizing pneumonia, and sepsis.
Hospitalized patients who are elderly, have serious symptoms, or have other medical problems are at highest risk of complications, so it is imperative that diagnosis and treatment are expedited by an experienced TelePulmonologist.
Sleep Disorders
Obstructive sleep apnea (OSA) is a serious sleep-related breathing disorder that is underdiagnosed, yet prevalence is expected to increase with growing rates of obesity — a major risk factor. Untreated OSA can cause significant cardiovascular issues like high blood pressure and stroke, and can worsen diabetes.
An Eagle TelePulmonologist has the expertise to identify symptom patterns that might elude other doctors and can order tests and provide treatment for these patients with the goal of controlling chronic respiratory problems at the root of sleep disorders.
How do patients typically react to telemedicine treatment?
How can telemedicine for pulmonology help your hospital?
“In working with hospitals, there’s a lot of listening going on,” says Dr. McCormick. “We help hospitals figure out what they need, and it’s often slightly different than what they might initially think,” he explains.
“In some cases, a double-boarded TelePulmonologist might be the perfect solution to handle the critical care cases as well as chronic cases on the floors,” he explains. “Maybe they need a TelePulmonologist on a 24-hour call schedule, for regular patient rounds and as a weekend backup for the local specialist.”
Eagle customizes every contract to meet the specific needs of your hospital and your patients. We get to the heart of your situation, to understand your staffing challenges, so your patients and staff get the greatest benefit.
Well-trained to adapt quickly to a hospital’s culture and processes, the TelePulmonologist will become part of your team — a friendly face, solving serious medical problems that require expertise for the best patient outcome.







