Is it time for a career transition? Find out what to expect from telemedicine physician jobs this year.
During the pandemic, telemedicine physician jobs “saved the day” in many hospitals. Telemedicine helped hospitals stay afloat in challenging times when more lucrative elective surgeries had to be postponed.
In 2020, healthcare was transformed by the pandemic. Hospitals of all sizes, in rural and metro communities, found an urgent need to connect with physician specialists. When restrictions on telemedicine were lifted by the Centers for Medicare and Medicaid Services (CMS), telehealth became the ubiquitous throughout the country.
Infectious disease specialists were in high demand, certainly. Hospitals also realized the need for specialists in ICU, Pulmonology and much more.
As a pioneer in telemedicine, Eagle was well-positioned to help these hospitals. Eagle has provided telemedicine providers since 2008 ― creating a platform to get both hospitals and remote physicians up-to-speed quickly while providing the highest-level of patient care.
The audio-video technology that enables the communication between the telemedicine provider and the patient/local team has proven highly effective in daily rounds, emergency and code blue situations.
In many cases, these Eagle provider serves as the sole specialist for that hospital, or serves as a backup for the local specialist. With telemedicine, hospitals can keep patients closer to home, instead of transferring them to a metro hospital 100 miles away.
As the new year 2021 approaches, let’s examine what the future holds.
5 predictions for telemedicine physician jobs in the upcoming year:
Eagle now provides coverage for 13 medical specialties — and the list of hospitals requesting these specialists grows daily. Here’s a snapshot of the potential ahead.
NICU & PEDIATRICS
Newborns and children require specialized care that may not be available in small community hospitals, especially on a 24/7 basis. Newborn Intensive Care Unit (NICU) support is necessary at a moment’s notice to evaluate and stabilize newborns, then determine the next steps in their care.
Pediatrics has been especially hard-hit by the physician shortage. In a nationwide survey by the Children’s Hospital Association, children’s hospitals were asked to name areas where pediatric specialist vacancies persisted for over a year.
Pediatric Neurology, Pain Management, Cardiovascular, and Otolaryngology were among the pediatric specialties with the highest wait times. The average wait time to see an Otolaryngologist is 2.3 weeks – one of the highest average wait times of surgical specialties.
Also, the demand for Pediatricians is expected to rise by 15 percent by 2026. These specialists will likely expect to earn an average salary of $212,000 a year, with a 5% increase per year.
A community hospital may have a pediatric hospitalist, a family medicine specialist, or a medical pediatric hospitalist who can provide daytime care for pediatric patients. However, if there are any coverage gaps (nights, weekends, holidays), the hospital must rely on locum tenens physicians at a high cost.
If a nurse assistant is trained in pediatric care, they need a pediatric specialist who will work with them. Without this on-the-spot care, there is a high likelihood the infant or child must be transferred, resulting in great family stress as well as transportation costs.
Telemedicine, increasingly, is coming to the rescue. For example, a Chicago health system is expanding its telemedicine platform to provide on-demand access to emergency pediatric services. Pediatricians at two suburban hospitals can access NICU specialists from a tertiary hospital via virtual care consults. The hospitals’ Emergency physicians will use the platform to connect with pediatric emergency medicine specialists.
This connection with Specialists provides the two hospitals with instant access to care — and reduces the need for costly and stressful transports to a tertiary hospital in downtown Chicago.
At Children’s Hospital Los Angeles, the efficacy of pediatric telemedicine care has been studied, with researchers determining that rounding conducted by offsite doctors ― with the assistance of remote-controlled robots ― was just as effective for NICU patients, compared to the regular on-site specialists.
Eagle’s Response: Eagle Telemedicine has expanded into Pediatrics and NICU to improve access to this specialty medical care. This unique service provides critical support for high-risk infants and hospitalized pediatric patients. Eagle’s TelePediatric Hospitalists provide coverage similar to TeleNocturnists who oversee adult patients on the night shift and on weekends.
Eagle’s TeleNeonatologists are available within minutes, day or night, every day of the year, to assist local providers in offering immediate care for the newborn in the NICU. This helps to avoid transfers to acute-care hospitals as much as possible, so the family can be nearby ― reducing the parents’ stress during a difficult time.
The TelePediatrician can see all the monitors in real-time, and the on-site staff will assist at every point. It’s as if the specialist is on-site, except that a child finds it ultra-cool the doctor is on the screen. The local providers learn exactly what next steps to follow, and very often can keep that child on-site, in their hometown hospital — close to home. No need for transfer 100 miles away, to the big hospital far from home, with all the scariness that involves.
MATERNAL-FETAL MEDICINE (MFM)
Severe maternal illness is on the rise in the United States, and women are dying in childbirth and from pregnancy-related causes at rates far greater than in any other economically advanced nation. States hit especially hard are Alabama, Arkansas, Kentucky, New Mexico and Texas.
For example, Alabama women die from pregnancy and childbirth complications at more than double the rate of women nationally, according to the National Center for Health Statistics at the Centers for Disease Control and Prevention. Alabama now ranks third highest in the nation in maternal death rates, behind Arkansas and Kentucky.
According to a CDC report, the severe maternal illness rate during delivery increased almost 200 percent from 1993 to 2014 across the US. This increase is due to increased rates of acute renal failure, cardiac disease, blood transfusion, and respiratory distress syndrome. A study of New Mexico found that women of color are more likely to be at risk for preterm birth, maternal and infant mortality — and that three out of five maternal deaths are preventable.
Researchers expect the rate of severe maternal illness to continue to increase. As women continue to become pregnant later in life, the chances for pre-pregnancy obesity, pre-existing chronic medical conditions, and cesarean deliveries increase, thereby increasing the rate of severe maternal illnesses.
Identifying at-risk women early in their pregnancy will potentially help provide timely medical care — and telehealth technology is at the heart of that program. This is expected to help prevent illness and death, shorten hospital stays, and reduce health care costs, researchers state.
An article in The New England Journal of Medicine outlined actions hospitals can take to “reverse the devastating trend in pregnancy-related deaths,” which included helping lower-resource hospitals to prevent the transfer of pregnant women requiring higher levels of maternal care. This is precisely the role that telemedicine can adeptly provide.
Telehealth improves maternal death rate: Rural states have used telehealth to improve maternal care management. The Montana Obstetric and Maternal Support (MOMS) program link OB/GYN experts with rural care providers to share expertise on a variety of topics affecting pregnant women such as Medication-Assisted Treatment (MAT) therapy and substance abuse counseling.
Researchers at the University of Arkansas for Medical Sciences (UAMS) are using a $228,000 federal grant to investigate how telehealth could improve Arkansas’ maternal death rate, which ranks fifth in the nation.
The research team will focus on using remote patient monitoring for pregnant women in rural areas where there are few health providers or resources. The objective is to determine if telehealth can improve rural healthcare for pregnant women with high blood pressure.
Maternal Mortality Rates by State
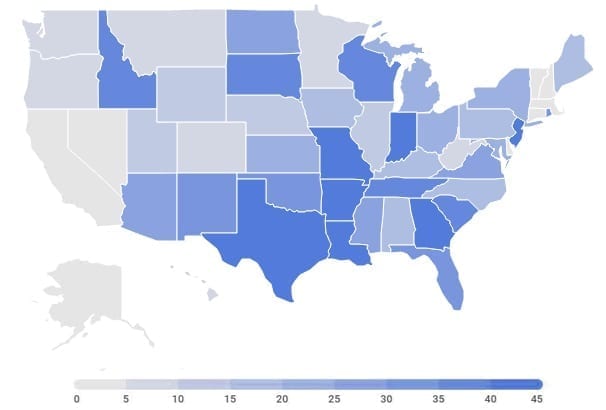
*Maternal deaths per 100,000 live births
Source: Ungar/Simon, USA Today, 10/26
The UAMS research team will recruit 50 pregnant women to test if maternal patient care can be improved using telemedicine video calls with UAMS maternal-fetal specialists and remote patient monitoring of blood pressure rates.
Eagle’s Response: Our Maternal-Fetal Medicine program is structured with Specialists who can quickly get on board with a hospital’s high-risk program. These Specialists form a strong relationship with on-site healthcare teams — physicians, nurses, and ancillary staff — to provide services these high-risk women need. They can jump on a patient consult 24/7/365, in the middle of the day or night, when needed.
This program dovetails well with the NICU telespecialty program, providing seamless coverage for mothers and their tiny babies, helping ensure the best possible start in life.
CHRONIC DISEASE MONITORING: In tandem with the growing obesity rate in this country, Eagle has seen a rise in requests for Endocrinology and Nephrology. While Eagle already provides Nephrology services on a limited basis, as well as Gastroenterology, there is discussion of adding Endocrinology and Dermatology.
Research shows that telehealth can be effective in treating diabetes patients. A year-long study conducted by the University of Nebraska and Wake Forest University found that a telehealth platform can help reduce the risk of diabetes in high-risk populations — by focusing on preventive measures to improve health and wellness.
Eagle’s Response: With the COVID-19 crisis, Eagle Telemedicine has seen strong interest in telehealth services — tele-Infectious Disease, Pulmonology, and ICU. The very nature of critical care medicine requires highly focused and meticulous medical specialists, and the procedures they perform are life-saving. The most favorable outcomes for these patients have been linked with high-intensity staffing, including a critical care specialist (an “intensivist”).
The intensivist has a pivotal role in coordinating the patient’s care, and therefore must be competent not only in a broad range of conditions common among critically ill patients, but also with the technological procedures and devices used in intensive care settings. Along with the intensivist, a pulmonologist is also necessary for critical treatment, as well as nurse practitioners and physician assistants who are also critical care specialists.
Tele-ICU reduces complications which often lead to readmissions, a key factor for Medicare penalties under The Hospital Readmissions Reduction Program (HRRP). The program focuses on unplanned re-hospitalization within 30 days for specific conditions including Acute Myocardial Infarction, Chronic Obstructive Pulmonary Disease (COPD), heart failure and pneumonia. CMS also measures hospitals on readmissions for any reason to the same hospital or similar acute care hospital.
With Tele-ICU, transfers to tertiary referral centers are decreased, as even the smallest rural hospitals provide the same valuable services to their communities as larger metropolitan hospitals. Tele-intensivists provide support to hospitalists and ICU nurses by being there with specialized expertise whenever they are needed. By the same token, they also provide value to community physicians who have privileges at their local hospitals.
Since the pandemic started, hospitals have contacted Eagle to prepare for coronavirus patients, and manage the care of patients with the virus. Eagle has been providing these services for years and expects the interest to continue growing.
In the first half of this year, the pandemic forced the medical community to adapt fast, using telemedicine as a stopgap measure to handle the emergency. As the months wore on, telehealth proved to build loyalty among patients and their doctors.
Doctor.com surveyed more than 1,800 patients about telehealth and the technology involved. The response was clear: Telemedicine is the future of healthcare. In early 2020, patient adoption was up 33% over the previous year.
Patients have increasingly shown their comfort levels with technology in setting appointments online. This trend continues, “mirroring today’s consumer experience: easy, immediate access to physicians, right from their smartphones — call it the “Uberization of healthcare,” according to a Medical Economics report.
Telemedicine saves patients over 100 minutes compared to an in-person visit, with each appointment in the comfort of their own home. In the Doctor.com survey, telehealth adoption is largely driven by convenience factors:
- Easy-to-use technology
- Online scheduling capabilities
- Immediate appointment availability
Instead of wasting half a day traveling to an appointment, a patient just hops on a 10-minute call before deciding on next steps or if a more extensive in-person appointment is warranted.
For physicians, the most promising implication relates to patient adherence. Telehealth removes barriers to care — while strengthening the patient/physician connection. Patients seem to recognize how telemedicine improves their healthcare: 93% report that they would use telemedicine to manage prescriptions, and 91% say that telemedicine would help them stick to appointments, manage prescriptions and refills, and follow wellness regimens as dictated by their doctor, reports Medical Economics.
Brick-and-mortar healthcare facilities are also evolving, with telemedicine being used in growing numbers of urgent care settings, micro-hospitals, and ambulatory care centers, as well as inpatient and outpatient surgery centers.
For example, Nutex Health, a Texas-based consortium of licensed, 24/7 micro-hospitals and freestanding Emergency Rooms, offers the convenience of a primary care provider’s office with the accessibility of a traditional ER. With over 25 locations across 8 states, including Oklahoma and Texas, the company is demonstrating how healthcare is evolving to meet consumer demand for convenience and proximity. Their team of board-certified emergency physicians provide superior patient care, along with quick treatment and drastically reduced wait times. (18)
In 2020, Eagle received requests for follow-up care ― inside of hospital-affiliated outpatient clinics ― for TeleNeurology, TeleStroke and TelePulmonology.
The trend toward telemedicine has been recognized by the American Medical Association’s vice president of digital innovation, who reported that even prior to the pandemic’s onset, telehealth visits and remote patient monitoring had doubled since a 2016 survey, increasing from 14% to 28% of physician respondents. (19)
The “AMA Digital Health Study” surveyed 1,300 physicians in 2016 and again in February 2019. Since the beginning of the COVID-19 pandemic, the use of telehealth rose dramatically. An estimated 60% to 90% of physicians were using some sort of telehealth services. About one-half were using telehealth for the first time.
“More physicians than ever have recognized digital health tools as an advantage for driving efficiency and safety in health care,” said Meg Barron, the AMA’s vice president of digital innovation.
The University of Virginia Center for Telehealth is developing a program to increase access to primary care and urgent care — as well as improve care in long-term care facilities, dialysis centers, clinics and other provider locations. A special program will improve access to 24/7 care in long-term care facilities via telemedicine consulting.
The UVA center has been a longstanding leader in the field, focusing on remote patient monitoring and intensive care. Most of the applications have been facility-based, until the arrival of COVID-19. Now, the center is using telehealth services to increase access to primary care and urgent care and to improve the efficiency of care with long-term care facilities, dialysis centers, clinics and other provider locations.
New telehealth goals have been set for inpatient and outpatient use, to improve access, triage and patient care management, reduce patient and provider COVID-19 exposure, conserve personal protective equipment, provide better access for primary care and specialty visits, and improve internal and external training.
The center is also using telehealth service to expand access to long-term care patients and facilities and has adapted remote patient monitoring developed for in-patient use to out-patient management of individuals with chronic conditions.
Amid this expansion of telemedicine, some barriers still exist that have slowed the progress. The physician’s ability to practice across state lines has been hampered.
During the pandemic, most states relaxed in-state licensing requirements for physicians. This allowed physicians to provide telehealth services in other states, to reach underserved rural and community hospitals. It also expanded access to many medical specialties that were critical to treating coronavirus patients — many that aren’t typically available outside metropolitan areas. However, the need for such access still exists.
Physicians, particularly specialists, must be able to work across state lines – and expansion of the Interstate Medical Licensing Compact (IMLC) is one possible solution.
By simplifying the physician licensing process, we can improve patient access to providers via telemedicine. One avenue is the IMLC, an agreement to streamline the licensing process for doctors outside their State of Principle License (SPL). Although just 29 states are participating in the IMLC, the potential is clear. It’s time to expand the IMLC and erase state licensing boundaries.
Eagle supports ILMC expansion to license physicians in multiple states. This is one more step towards solving the physician shortage and enabling a wider, easier adoption of inpatient telemedicine programs.
Since 2008, Eagle has proven (via experience) that virtual medicine is indeed a viable delivery model in hospital facilities. The Eagle model has also proven to be the most effective, compared to other platforms that utilize hard-wired beds connected to a “bunker” of computer screens that show alerts to doctors and nurses when a patient’s blood pressure drops, for example, or another significant change in condition is detected.
Eagle’s model is a team effort with on-site nurses and physicians who are “on the ground” monitoring ICU patients. This local team alerts Eagle’s team of intensivists (working from their home offices) via videoconferencing technology — and within just a few minutes, they are visible “on the cart” to diagnose the patient and recommend treatment options.
This has proven to be a more cost-effective approach and more proactive, compared to hiring locum tenens support. Tele-intensivists aren’t only available for emergencies, but they also can perform pre-emptive rounding. That is, rounding to spot potential problems before they occur.
The Eagle specialists are flexible; if a hospital only wants Tele-ICU coverage on weekends, we can provide it. Eagle provides the core team to share patient care management with onsite intensivists and/or hospitalists — via a cart with a video conferencing monitor.
All Eagle Specialists receive training, so they feel comfortable (and effective) in engaging with physicians via a remote monitor. And the technology has been fine-tuned since 2008 to ensure the highest-level audio/visual interaction, with the patient (and all bedside monitors) easily available.
Tele-ICU Coverage: The Eagle team covers the night and weekend gaps in ICU staffing, performing proactive Eagle Eye Rounding™ with ICU nurses to assess, triage and institute early treatment in patients with an acute decline in their clinical status. Our telemedicine intensivists can perform nursing unit rounds, as needed.
Or they can run an ICU, handling everything from floor call to attending rapid responses. Code Blue can even be managed virtually, with an Eagle Specialist calling the orders to the on-site team. Eagle has worked out the entire drill, so everyone on the ground (and virtual) knows exactly what to expect, how to proceed. We can report 100% positive outcomes with every Code Blue.
In fact, access to Specialists can help reduce 30-Day readmission rates and penalties. Simply by getting a second opinion, emergency staff can successfully discharge patients — greatly reducing readmission rates.
Physicians: It’s the Future of Medicine
If you’re a physician ready for a change from clinic work, looking forward to the future of medicine, telemedicine is an exciting frontier. Eagle started as a physician-led endeavor, providing hospitalist services for short-staffed facilities. Our founder foresaw the future of medicine in 2008, and we are on the cusp of his vision. It’s an exciting time to join Eagle Telemedicine — as we expand to meet the needs of healthcare throughout our country in rural, suburban and inner-city hospitals.
Take the first step! You can easily schedule a call with our…






