In the midst of the coronavirus crisis, hospitals in hotspot areas were overwhelmed and healthcare workers struggled to treat the thousands of patients across the country.
As the virus gradually worked its way into more communities, there came a tipping point. Patients were still coming into emergency departments for heart attacks and strokes, but hospitals needed rooms and resources to meet the demands of COVID-19 patients.
When a national emergency was declared, many of the needs for infected patients were met because The Centers for Medicare & Medicaid Services (CMS) telehealth rules were revised.
Guidance regarding non-emergency surgeries were altered, which was a mixed blessing for many rural hospitals. Many Critical Access Hospitals (CAH) and rural hospitals, already in financial crisis, were nearly pushed to financial ruin without elective surgeries. It meant beds standing empty and healthcare professionals with no patients to treat.
CMS Changes Could Save Rural Hospitals
In the early weeks, most rural hospitals saw few coronavirus patients. Then the inevitable occurred, and by late April, outbreaks were flaring in rural communities, the South and Upper Midwest. However, rural hospitals had no access to infectious disease specialists. Their patients deserve the same access that larger-city hospitals have, but were unable to bring in the necessary doctors.
Telemedicine was the silver lining. CMS telehealth rules changed dramatically compared to policies that governed these services in the past. This crisis has presented a huge opportunity to help rural hospitals during this crisis, and perhaps in the future.
It’s important to understand the nuances of this paradigm shift in telemedicine. So let’s take a look back at “how things were” and “how things have changed.”
Pre-COVID Telemedicine
In the pre-COVID days, CMS covered costs of telemedicine only under specific circumstances. For primary care telemedicine services, Patients were required to have an “established relationship” with the physician, within the past 3 years. That prevented some telemedicine professionals from stepping in during emergency and many other medical cases.
Hospital patients could only be seen in certain “originating hospitals” approved by Health and Human Services. Generally hospitals in designated Metropolitan Statistical Area (MSA) were unable to bill for professional fees on telemedicine visits. And, only patients seen in a hospital located in a Health Professional Shortage Area (HPSA) could be billed to Medicare for professional fees.
 Also, the attending physician was required to be an on-site to bill Medicare for H&P, so if telemedicine was involved in inpatient care, the billing options were complicated.
Also, the attending physician was required to be an on-site to bill Medicare for H&P, so if telemedicine was involved in inpatient care, the billing options were complicated.
Furthermore, while Medicare allowed US trained and licensed physicians to provide telemedicine services in US hospitals from locations outside of the US, the billing rules were structured in such a way that no professional fee reimbursement would be made if the physician was located outside of the US at the time of the visit. Many physicians who are located outside of the US for personal, family or other reasons are ready, willing and able to help patients in US hospitals, but this creates one more obstacle to providing needed medical services to rural hospitals
These restrictions have clearly limited the use of telemedicine — a service that we all believe can benefit patients in rural settings. When CMS telehealth rules were relaxed in March, this expanded our ability to provide services to a wider range of patients.
COVID-19 Crisis Changes
CMS recognized the urgency to expand use of telemedicine technology to help people who need treatment for COVID-19. The “3-year established relationship” requirement was eliminated. Also, CMS provided assurance there would not be audits of this stipulation.
The “originating hospital” and “attending physician” requirements have also been lifted. For the duration of the COVID-19 Public Health Emergency, Medicare will make payment for telehealth services furnished to beneficiaries in any healthcare facility — including any hospital across the country, which simplified billing. Nonetheless, there has been no change in the billing rules that require the physician to be sitting at a desk within the United State for professional fee reimbursement.
Immediately, we began hearing from hospitals interested in partnering with us to provide telemedicine for their patients. By shedding a spotlight on telehealth, CMS has enlightened the medical community about the benefits our services can bring to improve medical care.
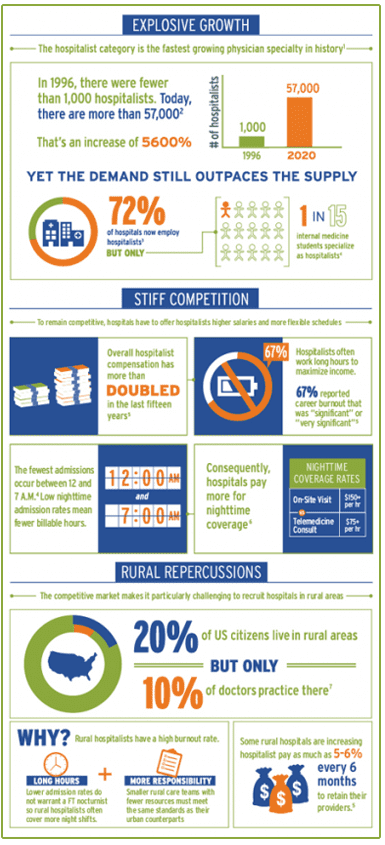
Why is rural hospital
staffing so difficult?
Physician shortages impact hospitals and patients across the country, but rural hospital staffing is even more difficult.
These hospitals depend on general practitioners, like hospitalists and nocturnist, to fill the gaps in specialist coverage.
We Advocate for Permanent Changes
As leaders in this industry, we believe that changes to CMS telehealth guidelines should be retained permanently and provide allowance for US trained and licensed physicians regardless of location to be reimbursed for telemedicine services rendered to patients in US hospitals. We also believe that making these changes permanent could greatly improve healthcare across the board — in struggling rural hospitals as well as suburban and metro hospitals.
Let’s examine the details:
Established relationship
This limits access to telemedicine hospitalists and specialists when a Medicare patient visits the hospital. Our own statistics clearly show that this is not necessary; a highly experienced physician can provide accurate diagnosis and treatment guidelines based on a “beamed in” visit with the patient.
When the appropriate diagnostic tests are conducted and results reported to the remote physician, there is the same accuracy in diagnosis — and treatment — compared to an on the ground hospitalist provider.
Rural and Critical Access Hospitals were already struggling to stay in business. The North Carolina Health Research Program reported that 19 rural hospitals closed in 2019. Indeed, the southeast has seen the most closures, with approximately 60% of rural hospital closures in the south. Most of these states did not expand Medicaid enrollment, an important source of revenue for rural facilities.
However, since 2010, 5% of rural hospitals have shut down, and the economic effects are immediate. One study found that when a community loses its hospital, per capita income falls 4% and the unemployment rate rises 1.6%.
A new Guidehouse analysis shows that this trend is likely to accelerate. According to the analysis, 21% of rural hospitals are at high risk of closing unless their financial situations improve.
Of these hospitals, 64% are considered highly essential to their communities based on an analysis of factors, including trauma status, service to vulnerable populations, geographic isolation, and economic impact.
Another problem: Fewer specialists are willing to work in rural areas. If they are willing to accept a position in a rural community, they may expect a higher salary, which the hospital cannot afford. Physicians can’t work 24/7/365, which is another hindrance to hiring good doctors.
These small hospitals are already struggling financially, yet their patients deserve the same access to medical specialists.
Originating site and attending physician restrictions
In the past, the telemedicine provider could be the attending physician — even if the provider is a specialist (think cardiologist) and the patient is in the ED. Problem is medical billing is complicated. If the ED doctor accidentally enters the telemedicine provider as the attending physician, the hospital can’t bill the professional fees.
Case Study: TeleHospitalists Provide Timeliness and Adaptability
Saint Luke’s Health System (SLHS) was no stranger to telemedicine when it called on Eagle to provide virtual hospitalist services in three of its 16 hospitals and specialty care institutes in November 2017.

Hospital Visits Via Telemedicine Nationwide
Telemedicine is a viable solution to many inequities that rural hospitals experience. We have known there is both a shortage and a maldistribution of doctors. Yet their patients deserve access to this high-level care.
Small hospitals rely on primary care physicians, like hospitalists, because they aren’t able to attract and retain specialists. They also don’t have enough demand for specialist services, like a neurologist, pulmonologist or infectious disease doctor to make full time practices. Even if the hospital is able to attract a specialist, there are still problems with covering the night shift and weekends.
This isn’t just critical to each patient, it is critical to our country, including the rural communities these hospitals serve. There is serious economic impact if a rural hospital closes, as these hospitals also serve as the area’s largest employer, which has a ripple effect driving additional businesses and jobs. We believe that implementing the CMS telehealth rules that has allowed for patients suffering from the coronavirus will help smaller hospitals increase revenue, improve access to care for patients and stay open.
Meeting the Challenge
Telemedicine has many applications in healthcare, and Eagle is ready to meet the demand. For those of us dedicated to providing these necessary services, it’s an exciting time. We believe the medical community will be encouraged by data that emerges from use of telemedicine during this crisis.
This is part of an upward trend we have witnessed in the past five years. As adoption of telehealth solutions or services has surged from roughly 54 percent in 2014 to 85 percent in 2019, indicating a higher level of acceptance and desire for telehealth solutions and services.
We stand with the American Telemedicine Association in advocating to eliminate artificial government barriers to telehealth, including geographic discrimination and restrictions on the use of telehealth in managed care. Our goal is to prevent new barriers to telemedicine, such as clinical practice rules that impose higher standards for telehealth-provided services than in-person care.
As we see in this COVID crisis, inpatient telemedicine is positioned to reduce health delivery problems, including provider shortages. Telehealth is fully capable of reducing health delivery problems, such as provider shortages. And, we continue to promote payment and service delivery models to increase consumer and payer value using telehealth.
Hospital patients deserve to have telehealth as a choice, as our services are shown to improve outcomes, convenience and satisfaction.