Many hospitals experience staffing challenges. While these challenges aren’t necessarily new, they have become more noticeable since the pandemic. Below, we share five of the reasons hospitals are experiencing staffing challenges and how telemedicine can provide support.
1. Hospital Staff Recruitment & Retention
Recruiting and retaining talent go hand in hand. A high turnover rate means hospitals spend more on recruiting expenses, training, benefits, termination costs, and hiring cycles instead of investing in other areas that could improve the overall work environment and increase the likelihood of retention.
Financial Impact of High Turnover Rates
In 2023, the national hospital turnover rate was 22.7%. In nursing, the vacancy rate was 15.7%, with a Recruitment Difficulty Index of 95 days, an 8-day jump from last year. Each percent change in RN turnover rates either costs or saves the hospital an average of $380,600.
Rural Hospital Recruitment and Retention
Retaining talent becomes even tricker for rural hospitals, where finances are already tighter. Mike Shimmens, Executive Director of 3RNET stated, “The number of primary care physicians available to serve in underserved areas is trending down while the demand is increasing. Finding physicians to practice in these areas of need is becoming incredibly more important and more difficult to do.” Unfortunately, rural hospitals are more likely to have staffing retention issues because they often can’t offer competitive benefits, which creates information deserts and a poor patient experience.
2. Staff Emotional Well-being
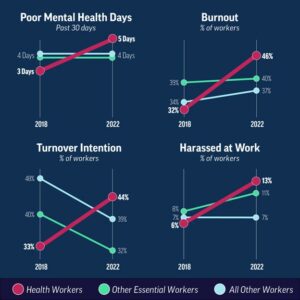
Staff emotional well-being is another challenge that many hospitals are struggling to tackle. In 2022, the CDC found that burnout was one of the top challenges hospitals faced. 46% of health workers reported feeling burned out often, a 14% increase from the 32% in 2018.
A Correlation Between Workplace Harassment & Burnout
One of the main reasons the CDC found healthcare workers struggling with anxiety, depression and burnout was increased harassment at work. Some of the solutions they suggest include modeling and supporting taking time off, including workers in decision-making, assigning senior leaders to promote staff well-being, training supervisors, ensuring adequate staffing and valuing worker safety and health.
High-stress Environments Take an Emotional Toll on Employees
No matter where you work, a high-stress environment will take an emotional toll. The quality of care patients receive is one way to tell if healthcare workers need a break. The Bureau of Prisons’ Health Services Personnel’s overtime costs increased by 64% in the first year of the pandemic. However, 80% of the federal prisoners rated medical care as “poor”. The increased yet poor quality of care indicates that these individuals were being stretched too thin.
3. Financial Resource Availability & Noncompetive Pay
When asked why workers quit their jobs, a 2021 Pew Research Survey showed that 63% of the respondents said low pay and no opportunities for advancement were factors in their decision.

The healthcare industry is no exception. The Insitute of Women’s Policy Research found a critical link between nurse supply and pay. Between 1996 and 2004, the median weekly earnings went up and down with the number of employed nurses. When pay increased, the patient-to-nurse ratio improved. An MGMA stat poll in 2022 found that 59% of medical staff turnover in 2021 was due to better pay and benefits elsewhere. The stats point to non-competitive pay as a factor in the physician shortage.
The Challange Behind Offering Competitive Wages
The challenge with offering competitive wages is that hospitals don’t have endless funds to throw at their staff. The continued rise of medical supply costs has made it increasingly difficult to budget higher wages and better benefits. It’s even more difficult for rural hospitals that don’t have as much to work with. They need to be strategic about the benefits they offer their staff so they can retain talent that best serves their patients.
How Telemedicine Relieves The Financial Burden Hospitals Face
Adding a telemedicine program can relieve some of the financial burden hospitals face. Telemedicine provides a high ROI by helping reduce hospital transfers, lowering turnover and physician burnout, eliminating locum support costs, increasing patient satisfaction and reducing the average length of stay.
4. Physician’ Relocation
There are a lot of different factors that go into the decision to relocate. Health Services Research published a 2017 study about physician migration. One interesting pattern they discovered was that federal programs, medical schools, and residency training locations play a role in a physician’s practice location. Additionally, they found that specialized physicians tend to move more than generalists.
Physicians Don’t Want to Relocate
PubMed found that 25% of physicians will move to a different county within five years. However, they often remain within the same urban or rural location for most of their career. The tendency for physicians to stay in the same vicinity is fine if the specialists you need are already in your area. However, if your hospital is looking to hire a specialist who would need to relocate, they will probably need more incentive to move. Hospitals in rural areas have a particularly tough time getting specialists to relocate to their area because they can’t compete with the amenities and salaries of urban hospitals and private practices.
Addressing Relocation Issues With Telemedicine
Telemedicine is one way that hospitals can improve their specialist offerings. It allows them to have specialists across the nation help their patients without needing them to move.
5. Using Travel Nurses to Fill Staffing Gaps
Travel nurses have been around since the 1980s, providing needed short-term staffing gap support. However, the use of travel nurses isn’t a perfect system. Some issues around travel nurses include higher costs, staff alienation, recruitment issues, and legal headaches.
While temporary nursing positions grew by 40% in 2021, the need for temporary workers in the healthcare industry has decreased since COVID-19 hospitalization rates have stabilized and relief funding has stopped. The demand for registered travel nurses decreased by 42% from January to July 2022.
While the use of travel nurses has decreased, the need to cover staffing gaps hasn’t gone away. In 2021, the AAMC projected primary care shortages would range from 17,800 – 48,000, and specialist shortages would range between 21,000 and 77,100 by 2034.
Using Telemedicine to Cover Staffing Gaps
When you use Eagle Telemedicine, you can add remote staff support to your team without the high costs of employing travel nurses. Eagle’s telehealth staff supports your team and integrates with on-site staff whenever you need them. Eagle staffing gap services include TeleNocturnists, surge protection and NP/PA backup.
The five factors above have made retaining medical staff a struggle for hospitals. However, there are solutions available that can alleviate these pain points and help hospitals provide patients with the quality care they deserve. One notable solution is the addition of telemedicine services. Connect with Eagle today and determine the best solution for your hospital.
Photos: https://www.cdc.gov/vitalsigns/health-worker-mental-health/index.html#:~:text=The%20study%20showed%20how%20symptoms,compared%20to%2032%25%20in%202018.
Related Posts:
5 Telemedicine Long-term Benefits for Hospitals
Solving The Financial Burden with Telemedicine